Maladies et pathogènes
L'agence focalise son action sur la recherche sur le VIH/sida, les hépatites virales, les infections sexuellement transmissibles, la tuberculose et les maladies infectieuses émergentes (en particulier les fièvres hémorragiques virales, les arboviroses et les infections respiratoires émergentes, dont la Covid-19).
Dernière mise à jour le 22 mars 2023

Arboviroses
Les arboviroses sont des maladies dues à des arbovirus (arthropod-borne viruses), c’est-à-dire des virus qui sont transmis aux humains…
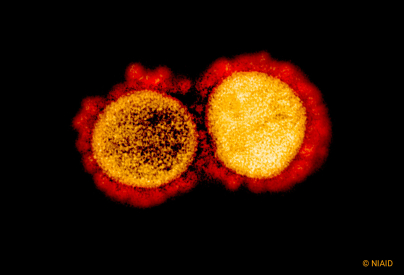
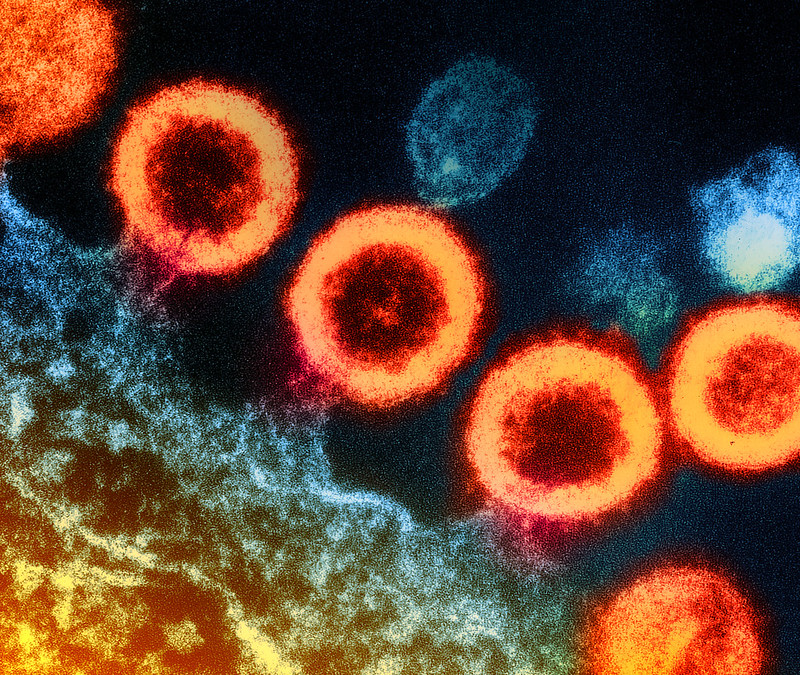
Covid-19
Apparu en décembre 2019 à Wuhan, au centre de la Chine, le coronavirus SARS-CoV-2 s’est très rapidement propagé à l’ensemble de la planète.
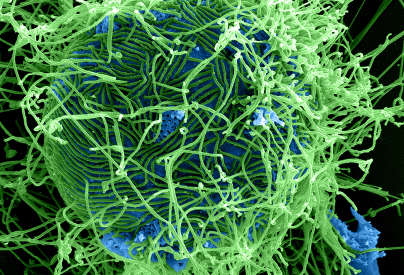
Fièvres hémorragiques virales
Les fièvres hémorragiques virales (FHV) regroupent différentes maladies (Ebola, fièvre de Lassa, de Marburg…).
Hépatites virales
Les hépatites virales sont des inflammations du foie causées par un ou plusieurs virus (A, B, C, D et E).
Infections sexuellement transmissibles (IST)
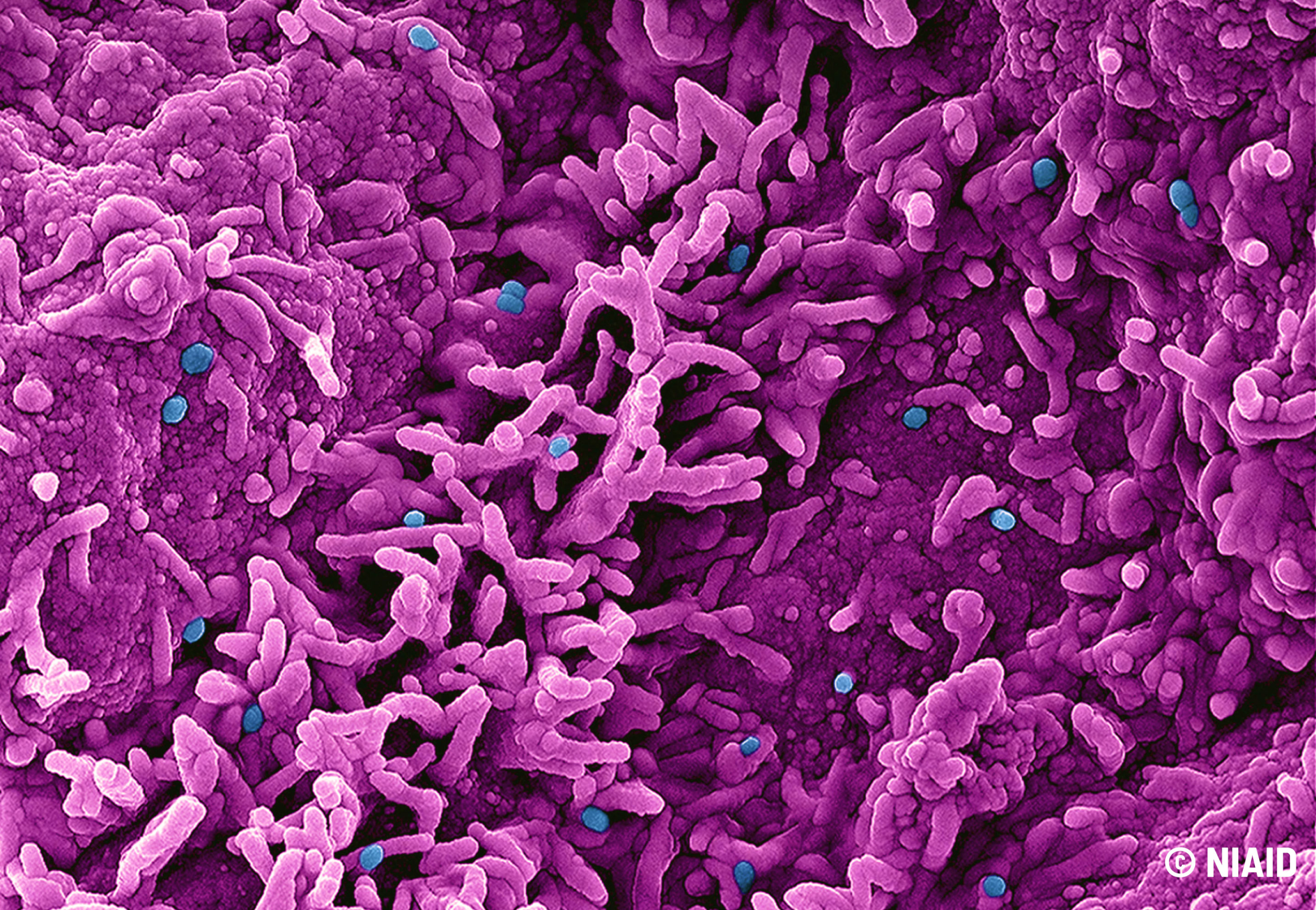
Parmi les infections sexuellement transmissibles (IST), la plupart sont dues à des bactéries, des parasites ou à des virus.
Mpox
Mpox (anciennement appelé « variole du singe » ou « monkeypox ») est une maladie circulant depuis des décennies en Afrique de l’Ouest et du centre.
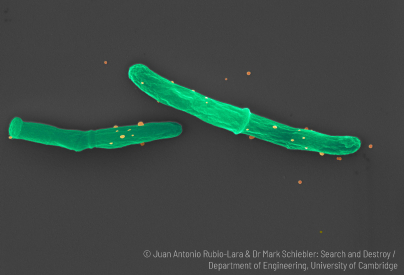
Tuberculose
La tuberculose est l’une des maladies infectieuses les plus meurtrières. Chaque jour, près de 28 000 personnes la contractent et plus de 4 100 personnes en décèdent d’après l’OMS.
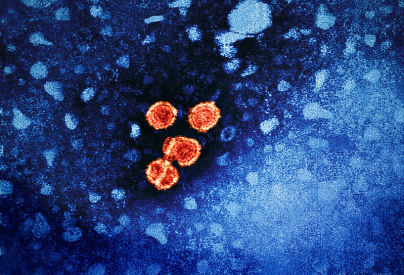
VIH
Le virus de l’immunodéficience humaine (VIH), responsable du sida, touche environ 38 millions de personnes dans le monde d’après l’OMS.
